SI Joint Fusion With Stereotactic Navigation
Joshua E. Heller, MD, MBA
Aria Mahtabfar, M.D.
Thomas Jefferson University Hospital
Patient History
68 year-old female with history of low back, and left greater than right hip/pelvic pain with initial onset in 2014. She has a history of stand-alone L5/S1 ALIF in 2016, which saw minimal improvement in her symptoms. Subsequently, the patient underwent B/L SI joint fusions. Immediately post-op the patient had worsening hip and pelvic pain, as well as bilateral lower extremity weakness. CT scans were performed, which showed that 2/4 threaded cages were anterior and superior to the sacrum in the location of bilateral L5 nerves. She underwent immediate revision surgery with removal of malpositioned implants and placement of fixation screws across her SI joint. Patient presents reporting continued back, left greater than right hip/pelvic pain with slow improvement of bilateral foot weakness.
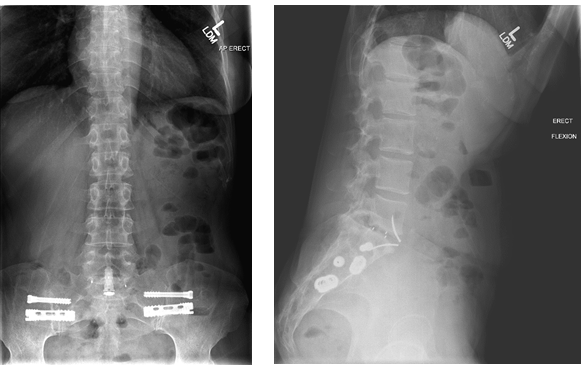
Pre-OP Imaging:
Diagnosis
Given the continued symptoms, positive provocative testing, and adequate relief after diagnostic injection, the patient was diagnosed with SI joint dysfunction, and recommended to undergo a left SI joint revision fusion.
Treatment
The patient underwent revision left SI joint fusion with stereotactic navigation, removal of stabilizing screw and placement of iFUSE implants with open decortication and fusion of the SI joint using BMP and boss retractor
Outcome
6 weeks post-op from surgery patient with dramatic improvement and near resolution of her pre-operative symptoms. 3 months post-op patient reporting no pelvic or hip pain, with full return to work and functional independence.
Discussion
While this patient thankfully made an impressive neurologic recovery after her initial SI joint dysfunction, the pain and symptoms continued to be debilitating. Recognizing and diagnosing continued SI joint dysfunction proved to be vital in this case, which may be confounded by the history of prior lumbosacral fusion and low back pain. Interestingly, in her initial evaluation of SI joint dysfunction, the patient had never undergone provocative testing or diagnostic injections. Furthermore, a minimally invasive open decortication with BMP was pursued to increase the potential for arthrodesis given the patient’s history of pseduoarthrosis
Relevant Images
Prior to immediate revision surgery
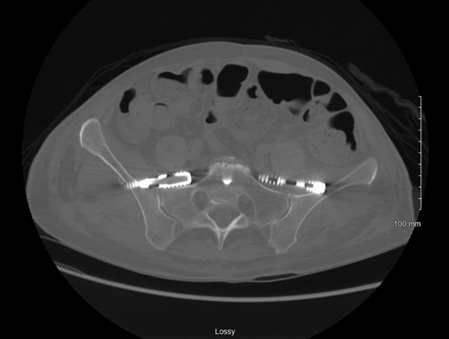
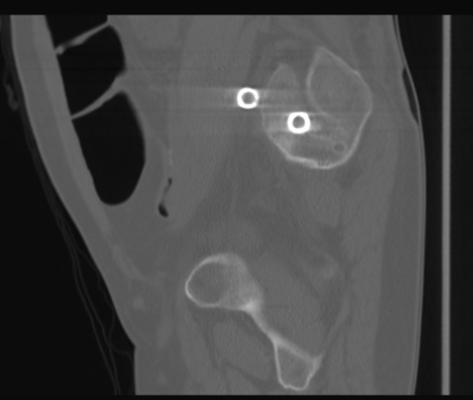
Prior to immediate revision surgery
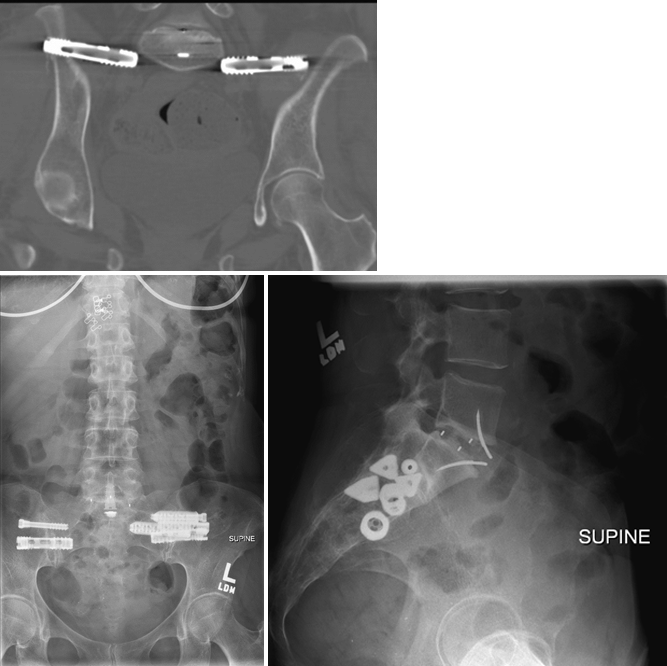
Post-op from L SI joint revision fusion